BVH Revenue Cycle Management
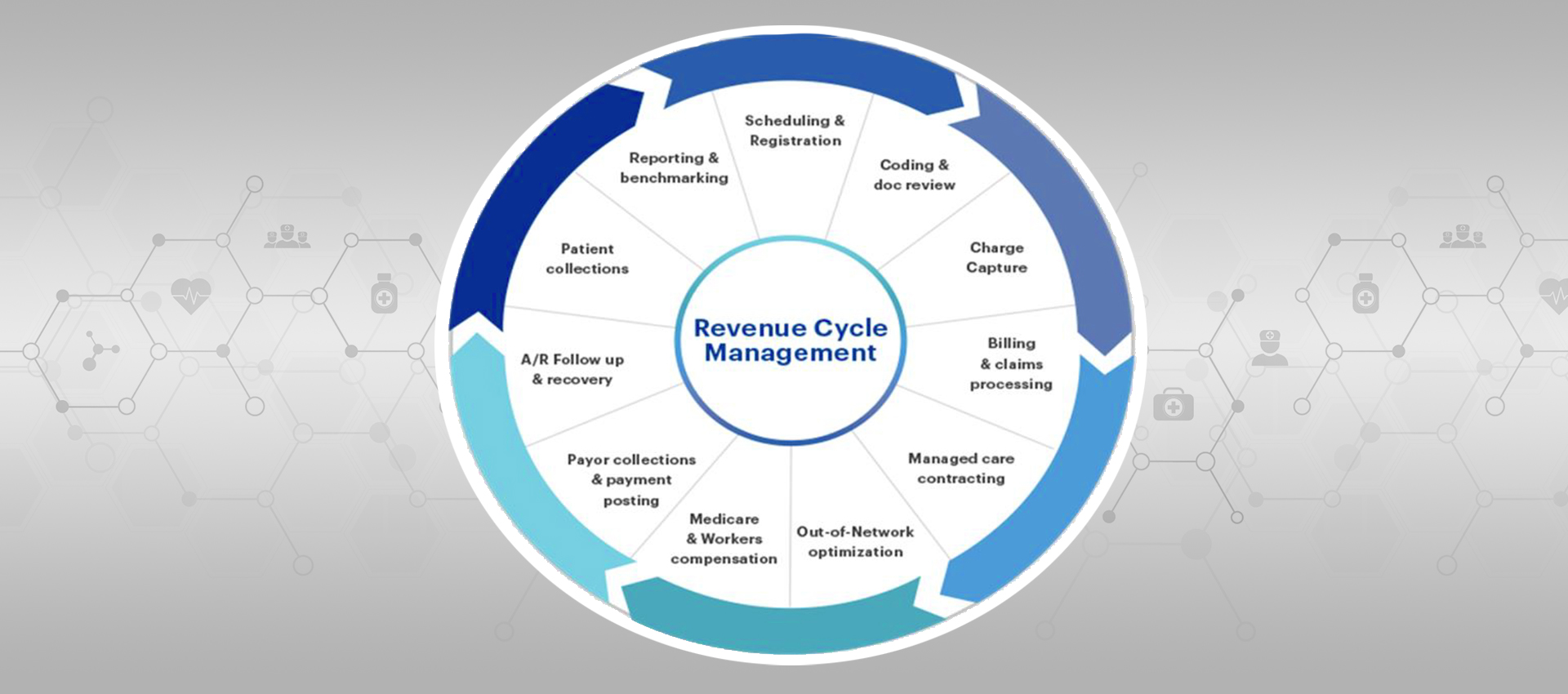
Creating sustainable margins for your inpatient and outpatient services requires a proven strategy and streamlined revenue processes. The Boa Vida Healthcare Revenue Cycle Management team of experienced professionals can help you design and implement your healthcare reimbursement transformation by assessing critical policies, procedures, practices and processes. Boa Vida will leverage historical data to determine essential functions, including patient access, charge capture, clinical documentation, denials management and operational business workflows.
Boa Vida Healthcare is a national healthcare organization that owns and operates four hospitals and 20 clinics. Boa Vida has designed and implemented a healthcare model that substantially improves and expands a community’s healthcare services. Comprised of an interrelated group of companies, Boa Vida focuses on healthcare solutions for payors and providers.
Revenue Cycle Transformation
Healthcare organizations have ongoing stress to increase organizational margins, more than just a quick cash infusion—it is imperative to create a sustainable solution. Our experienced professionals can help you accelerate revenue, redesign processes, and implement the transformation to increase revenue and efficiency and reduce denials that last long-term.
- CDI
- Charge Capture
- Charge Capture Assessment
- Managed Care Contracting
- Revenue Cycle Assessment
- Denials Management
- Pricing Strategy & Transparency
- Hospital Chargemaster Improvement
- Coding & Billing Compliance
- Payor Contract Management
- Post-Implementation Revenue Cycle Services
- Revenue Cycle Analytics & Reporting
- Billing and Follow-Up Services
- Patient Access Management
- Registration
- Scheduling
- Credentialing
- Specialize in Rural Healthcare Systems, CAH, RHC
- Increase Revenue through community engagement
A Proven Partner for Healthcare
Our programs help provide complete visibility into your clinical documentation and coding so you can quickly spot opportunities to improve reimbursements, manage risk and resolve operational challenges like denials and billing delays. Boa Vida is a leading provider in transforming RCM services with built-in Cloud-based Meaningful Use Stage-3 certified EHR and PMS technology. It provides efficient, responsive and accountable billing implementation. Back-office services give more than 98% first-pass claims submission and efficient A/R follow-up/denial management at very competitive rates.
Submissions of Claims
Submission of claims is vital in the overall RCM process because the reimbursement directly depends on it. There are possibilities that repayments will be reduced or outright denied if this process is mismanaged. Once the biller prepares the claims and files with the insurance companies via EDI clearinghouse. The clearinghouse applies scrubbing technologies to ensure that the claims are clean and free from errors.
Co-Payments and Deductibles
Each health plan mandates a deductible, a co-payment, and co-insurance. Some patients have high and some have low deductibles, according to their insurance. Whatever the amount is, it is essential that patients clearly understand the responsibility to pay the providers’ copays.
Reimbursement for Services Provided
It is the most awaited step in the entire process. It is time for the insurance company to pay up for your services. The insurer matches the procedures with their charges under the coverage limit. If the bills are appropriate, the process of reimbursement becomes smoother and returns maximum payments. However, in erroneous claims and incomplete patient information, or any other issues, the denials are inevitable.
Charge and Code
When the patient visits the provider’s facility, the visit gets transformed into a set of codes. There is a high probability of human error in these charges and codes. Therefore, it is vital that professional medical coders are present to manage this activity. The codes must follow a particular set of rules and concur with the CPT guidelines and the latest ICD-10 coding system.
Patient Precertification or Pre-Authorization
When a patient comes in, they undergo pre-authorization. The provider’s office pre-authorizes the patient for specific treatments and prescriptions of drugs. Pre-authorization is the step where the patient or the insurance companies must decide whether the prescription of the drugs, procedures, services or equipment is medically necessary or not. Based on the decision, insurance companies will reimburse for the services provided.
The pre-authorization process is repetitive and needs continuous verification each time.
It is always a good idea to double-check any doubts related to coverage with the insurance company. The pre-authorization phase faces exceptions in case of a medical emergency.
Manage Denials
The claims, rejected or denied, are resubmitted soon after they are restored with coding mistakes. The resubmissions process demands crucial screening with a pointer on the latest coding guidelines. Also, every minute detail is checked against the patient profile.
Boa Vida is a leading provider in transforming RCM services with built-in Cloud-based Meaningful Use Stage-3 certified EHR and PMS technology. It provides efficient, responsive and accountable billing implementation. Back-office services give more than 98% first-pass claims submission and efficient A/R follow-up/denial management at very competitive rates.
Eligibility and Verification of Insurance
This process is crucial. Therefore, it is essential to confirm the eligibility and verification process to avoid reimbursement issues. Once the patient goes through the care delivery, the Explanation of Benefits (EOB) statement incorporates all the details of the services or treatments paid on their behalf by the insurance company. Verification will prevent a patient from being blindsided with additional out-of-pocket expenses.
340B Program, Pricing & Compliance
Boa Vida assists providers with all aspects of the 340B program, including independent audits, operational consulting, and continual monitoring. We can help you improve your program’s financial strength and compliance levels.
Boa Vida’s 340B team has the expertise to provide operational knowledge and recommendations that help covered entities increase savings and maintain compliance. Our team has experience with most split-billing vendors, wholesalers and billing systems and we understand the complexities of building and maintaining a 340B program.
As the 340B Drug Pricing Program expands, it is under continued scrutiny for payment reform and legislative changes. Boa Vida’s Washington, D.C., perspective on industry trends and challenges, along with our extensive health care experience, provides you with timely legislative updates and solutions for your 340B program.
Boa Vida Revenue Cycle Services Designed to Fit Your Needs
Boa Vida offers comprehensive and flexible healthcare Revenue Cycle Management services and technology solutions to help you reduce costs and improve your bottom line. Whether you need flexible resourcing or full back-office support, our experts can review your current revenue cycle practices to identify opportunities to improve productivity, claims and cash management and accounts receivable.
We leverage best practice workflows and technology automation to improve cash flow and enhance profitability. Technology is critical for improving efficiencies and automating processes. The Boa Vida Revenue Cycle platform for Clearinghouse and eligibility management will increase clean claims submission rates and speed up cash collections simply by managing electronic claims effectively.
Our highly trained account managers go above and beyond to help you and your office staff!
At Boa Vida Healthcare, we pride ourselves on our outstanding customer service. Our team of experts is always available to answer any questions that your team may have. We follow up on all claims promptly, and we continue to work on both primary and secondary claims until they are paid!
 The Boa Vida Revenue Cycle Process for Hospitals and Clinics
The Boa Vida Revenue Cycle Process for Hospitals and Clinics
The Boa Vida team of experts apply the best practices to the following elements of the revenue cycle process: Patient Precertification, Eligibility and Verification of Insurance, Charge and Code, Co-payments and Deductibles, Submission of the Claims, Reimbursement for the Services Provided, Manage Denials, 340 B Program, Pricing & Compliances. Designed to fit your revenue cycle needs!
The Boa Vida Healthcare Revenue Cycle Management team of experienced professionals can help you design and implement your healthcare reimbursement transformation by assessing critical policies, procedures, practices and processes. Let our team complement your team!




